What You Need to Know About Gluten & Celiac Disease
Celiac disease is an autoimmune disease that flares with even an invisible amount of gluten contact via mouth, skin, and even lungs. About 2 million Americans suffer from celiac disease, with that number slowly rising each year, especially amongst children. This works out to about 1% of the general population, and up to 10% for those with an affected immediate family member. This is different from non-celiac gluten sensitivity (6% of Americans) and other wheat-related disorders, because of the way the immune system responds. All gluten-related disorders can be genetic, and there is increased likelihood of non-celiac gluten sensitivity in family members of those with celiac.
Gluten, a protein in wheat and certain grains, is now found nearly everywhere in our modern world. It is not only in flour-based foods such as pasta and bread, but it is also used as a filler in foods such as meat substitutes, medications, and supplements; it forms the basis of Play Doh; and it’s even in water-activated envelope and stamp adhesive (don’t lick it!). Additionally, gluten is used in body products such as toothpaste and shampoo, and it can find its way into “gluten-free” foods such as grains or restaurant meals through cross-contamination and poor food handling practices.

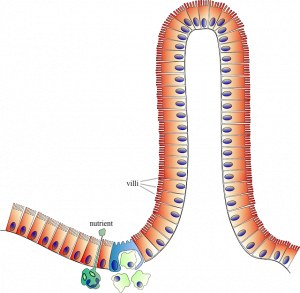
With celiac, the immune system sees gluten and in response attacks the villi, or finger-like projections, that line the small intestines. This creates chronic inflammation that leads to tissue damage – the immune system flattens the villi with its attack, and the villi can no longer release digestive enzymes to break down food or absorb nutrients through the intestinal wall and into the bloodstream for delivery throughout the body. Aside from causing diarrhea or constipation, gas and bloating, nausea and vomiting, abnormal stools, or gastrointestinal pain on gluten exposure, people with celiac are more likely to suffer from nutrient deficiencies, which could ultimately result in conditions such as anemia and neuropathy, as well as weight loss, osteoporosis, or inhibited growth in children.
The autoimmune component of celiac is critical to address given not only the immediate consequences of gluten exposure, but also the resultant impact of long-term immune system dysfunction: The body becomes so busy trying to fight the perceived danger from every gluten exposure that it is unable to always clear actual infections, or may even develop a misguided response to other tissues in the body. This can lead to over- or under-reactions to illnesses, low-grade simmering infections in tissues, and even the eventual development of multiple autoimmune diseases if not addressed. You can learn more about autoimmune disease in general here: Autoimmune Diseases.
Celiac disease can be tested for via blood, but one needs to have eaten gluten within several weeks of the test in order to obtain results. We NEVER recommend eating gluten for the sole purpose of testing, and do encourage you to obtain a celiac test before going gluten free if you suspect this is a problem for you. To test for celiac, you can ask your physician to order a celiac panel, or we can order you a Wheat Zoomer that assesses for many different wheat-related disorders, including celiac markers (however, we do not make a diagnosis, only confirm if gluten is an issue for you). The absolute gold standard for diagnosing celiac is a biopsy, but it can take a decade to sustain enough villi damage to have obtain the diagnosis this way. One reason to find out for sure if you do have celiac is that if it’s an issue for you, you will need to take extra precautions when eating at a restaurant or checking labels on prepackaged foods, or ensuring your child’s eating surface at school is cleaned appropriately. And of course, since there is a genetic component, it may be helpful to determine if celiac runs in the family.
When strictly avoiding gluten, it’s important to read labels as well as look for gluten free certifications. These are some of the more common ones:
If you do have celiac and choose to eat at restaurants, having a toolbox on hand can be protective against accidental exposures. One helpful product is a special digestive enzyme called DPP-IV, which helps to break down gluten in case of accidental exposure. A few of our DPP-IV-containing favorites include Microbiome Labs Wheat Rescue or Dr. Tom O’Bryan’s E3 Advanced Plus. These products don’t allow us to indulge in a plate of glutinous pasta or a crusty roll, but do give us extra support and peace of mind in case of any hidden sources of gluten. Another product is gluten testing strips, such as EZ Gluten, which allow you to sample your food and beverages to quickly detect the presence of gluten before you eat it. This could truly make all the difference in the life of a celiac or someone who’s highly allergic or sensitive to gluten.
Needing to go gluten free? We can help you adapt your lifestyle to a new celiac or non-celiac gluten sensitivity diagnosis, or rebalance autoimmune dynamics in the body. This can help you feel better, absorb nutrients better, and even reduce the likelihood of acquiring a second autoimmune diagnosis. If you are interested in being supported, please sign up for a complimentary session to learn more.


